Introduction
Long Covid (LC) and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) are both post-viral conditions which have similarities in symptom presentation and management. However, patient experience between these NHS pathways is uneven. LC services, enabled through ring-fenced funding from NHS England, were rapidly introduced across the Buckinghamshire, Oxfordshire and Berkshire West Integrated Care Board (BOB ICB) region in 2020. These implemented new multi-disciplinary models to treat the complex needs of patients leading to reductions in recovery time and improved clinical and NHS resource utilisation. By comparison, ME/CFS patients often face long waiting times, fragmented care, multiple referrals and extensive investigations before receiving appropriate management.
Similarities in symptom presentation present an opportunity to apply the same structured approach to ME/CFS services as has been implemented for LC. Establishing a clear pathway, incorporating multi-disciplinary team (MDT) assessments and providing access to a jointly provided range of rehabilitation support, could significantly improve patient care and resource efficiency.
In March 2024, the BOB ICB Integrated Respiratory Delivery Network requested support from Health Innovation Oxford and Thames Valley (HIOTV) to develop a case for change by exploring key areas. One of the primary considerations was service integration and resilience, with the aim of combining LC and ME/CFS resources to strengthen service delivery, enhance patient support and increase overall capacity. A more efficient use of the workforce, particularly multi-professional healthcare practitioners (HCPs), could optimise service provision and allow a broader patient population to be served effectively.
“We value the comprehensive coordination, analysis and evaluation that Health Innovation Oxford and Thames Valley have provided as our system partners. The Long Covid and ME/Chronic Fatigue Syndrome integrated care model design and evaluation provide key insights and recommendations for services within Buckinghamshire, Oxfordshire and Berkshire West to progress service integration which has the potential to reduce disparities and improve patient care, workforce sustainability and system efficiency.”
Paul Swan, Integrated Respiratory Delivery Network (IRDN) and Long Term Conditions Oxfordshire Lead, BOB ICB
Method
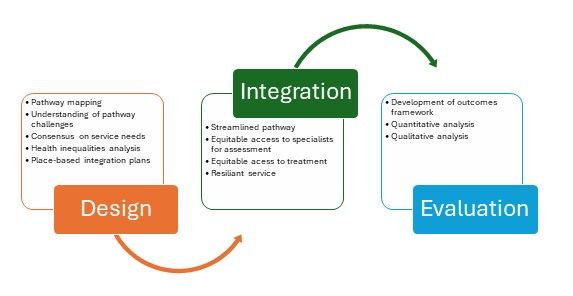
HIOTV used a real-world mixed methods approach which consisted of two strands:
- Design This helped to understand the current service challenges, co-design and implementing a place-level integrated model.
- Evaluation This assessed the impact of the integrated model as it was implemented.
The evaluation of implementing an integrated system covered:
- Designing an integrated pathway using a flexible place-based approach, recognising the variability in existing service provision, resource availability and commissioning arrangements across different areas
- Conducting analysis to compare the differences in care received by patients from LC and ME/CFS services
- Conducting a health economics analysis looking at both whole system costs and patient outcomes for LC and ME/CFS services
- Conducting staff surveys to provide in-depth insights into integration and on their perspectives of working for the services
- Conducting semi-structured interviews with patients to explore their experience of current services and views on integration.
The qualitative and quantitative data was analysed separately and integrated, allowing for comparisons and joint interpretation to provide richer insights.
Results
The evaluation identified significant challenges with the current service provision, notably inconsistent referral pathways, long waiting times, health inequalities and fragmented data collection.
It concluded that integrating LC and ME/CFS services could lead to:
- Better patient experience and equity – improving patient flow and efficiency of referral pathways leading to better access and reduced service inequalities
- Improved workforce capacity, resilience and experience – easing pressure on staff and increasing access to specialist collaboration and medical experience through expanding MDT working, with staff reporting an increase in job satisfaction
- System-wide cost-saving and productivity benefits – streamlining referral processes and reducing service duplication by integrating LC and ME/CFS services could reduce costs by 5.3% and increase patient capacity by 18%, predictive modelling suggests.
Summary and recommendations
Integration of the services presents an opportunity to enhance patient care, strengthen workforce capacity and improve overall system efficiency. Early integration efforts have yielded positive outcomes, but continued evaluation, strategic planning and sustainable investment will be essential to ensure long-term success.
We propose these recommendations to address existing challenges and build on the early successes:
- Establish a single point of referral: Standardise referral pathways and diagnostic criteria to ensure timely and equitable access
- Enhance access to MDT and medical support: Optimise resource allocation to provide patients with comprehensive, multi-disciplinary care
- Align assessment and treatment timelines: Improve consistency and service capacity
- Ensure sustainable workforce and funding plans: Implement long-term workforce strategies and secure ongoing financial support
- Expand and standardise workforce training: Develop targeted training programmes to enhance staff skills in managing LC, ME/CFS and related conditions
- Improve GP education and referral awareness: Provide structured GP training to ensure timely and appropriate referrals
- Address health inequalities: Implement targeted outreach and digital inclusion strategies to improve access for underserved populations
- Enhance patient communication and service clarity: Standardise information delivery to improve patient expectations and engagement
- Standardise data collection and monitoring: Develop a unified data framework to track key metrics, monitor health inequalities and support continuous service improvement.

